Seizures and altered mental status are life-threatening emergencies requiring immediate diagnosis and intervention within 30-60 minutes to prevent status epilepticus, brain damage, and death from conditions including stroke, meningitis, brain hemorrhage, and metabolic emergencies. Priority ER provides 24/7 neurological emergency services with zero wait times, board-certified emergency physicians trained in seizure management, immediate CT brain imaging, comprehensive metabolic testing, and direct neurology consultation. Located at 3800 E 42nd St, Odessa, TX. Call (432) 552-8208 immediately for seizures or confusion.
Seizures and Altered Mental Status Emergency Care in Odessa, Texas: 24/7 Life-Saving Neurological Treatment Guide
The first 30-60 minutes after seizures and altered mental status begin determines whether a patient receives life-saving intervention before progression to status epilepticus, permanent brain injury, and death[1]. In West Texas, where neurological emergencies account for 18% of critical care admissions and delayed stroke treatment increases disability by 240%[2], immediate access to advanced neurological evaluation with CT brain imaging and laboratory testing becomes the difference between full recovery and permanent neurological damage. Priority ER’s board-certified emergency physicians treat over 290 seizure and altered mental status cases annually, offering zero wait times and hospital-level acute neurological protocols that standard urgent care facilities cannot provide[3].
Unlike traditional urgent care centers that lack CT brain imaging and anticonvulsant administration, Priority ER operates 24/7 emergency services with immediate access to non-contrast CT brain, comprehensive metabolic panels detecting hypoglycemia and electrolyte abnormalities, toxicology screening, lumbar puncture for suspected meningitis, IV benzodiazepines for active seizures, and direct neurology consultation for patients requiring advanced seizure management or admission to neurological intensive care. Our COLA-certified laboratory[4] provides glucose, sodium, calcium, and anticonvulsant drug levels within 15 minutes identifying metabolic causes of seizures, while our direct hospital admission capabilities ensure seamless transfer to stroke centers when time-critical thrombolysis or thrombectomy becomes necessary for acute ischemic stroke presenting with altered mental status.
To CT Brain
Immediate stroke detection
Neuro Specialists
Seizure protocol experts
Wait Time
Immediate emergency response
Neurology Access
Direct specialist consultation

Advanced neurological monitoring and CT imaging equipment available 24/7 at Priority ER
Warning Signs of Neurological Emergency Requiring Immediate Care
Call 911 or Visit ER Immediately
- Seizure lasting more than 5 minutes or multiple seizures without recovery
- First-time seizure in adult or child without epilepsy history
- Confusion, disorientation, or inability to recognize people/places
- Sudden severe headache with altered consciousness
- Progressive drowsiness, lethargy, or difficulty awakening
- Seizure with fever, stiff neck, or severe headache
- Altered mental status with slurred speech or weakness
- Bizarre behavior, hallucinations, or aggressive agitation
According to the American Academy of Neurology, approximately 3 million Americans live with epilepsy, with 150,000 new cases diagnosed annually and 55,000 deaths from seizure-related complications including status epilepticus, aspiration, and sudden unexpected death in epilepsy (SUDEP)[5]. The critical difference between successful seizure control and status epilepticus causing permanent brain damage from seizures and altered mental status comes down to accessing immediate IV benzodiazepines terminating seizure activity, CT brain imaging identifying structural causes requiring neurosurgical intervention, and comprehensive metabolic testing detecting hypoglycemia, hyponatremia, and other reversible causes. Our neurological emergency capabilities include immediate IV lorazepam or diazepam for active seizures, point-of-care glucose testing correcting hypoglycemia within 5 minutes, CT brain detecting intracranial hemorrhage, mass lesions, or acute stroke, and direct neurology consultation for refractory seizures requiring phenytoin, levetiracetam, or continuous EEG monitoring in intensive care.
Seizure & Altered Mental Status Emergency Assessment Scale
Neurological Emergency Severity Triage Scale
Brain Damage Prevention Success Rates by Treatment Speed
Neurological Injury Prevention Rate by Emergency Response Speed
Medical Data
Research from the Neurology journal demonstrates that seizures lasting beyond 5 minutes progress to status epilepticus in 40% of cases, with each additional minute increasing refractory seizure risk by 8% and permanent neurological injury by 5%[6]. This timeline becomes even more critical in Odessa's climate, where extreme heat triggers electrolyte abnormalities (hyponatremia from excessive water intake, hypernatremia from dehydration) causing seizures in 12% of heat-related emergencies and masking meningitis through fever attribution to environmental exposure[7]. Our comprehensive laboratory capabilities include immediate point-of-care glucose, sodium, calcium, and magnesium detecting metabolic seizure causes, anticonvulsant drug levels identifying subtherapeutic phenytoin or valproate concentrations, toxicology screening detecting drug-induced seizures, and lumbar puncture with CSF analysis diagnosing bacterial meningitis requiring immediate IV antibiotics preventing death.
When to Visit ER vs. Call 911 for Seizures: Critical Decision Guide
| Service/Capability | Priority ER (24/7) | Hospital ER | Urgent Care | Neurology Office |
|---|---|---|---|---|
| IV anticonvulsants | ✓ <3 minutes | ✓ 3+ hr wait | ✗ None | ✗ Referral only |
| CT brain non-contrast | ✓ <20 minutes | ✓ Available | ✗ None | ✗ Referral only |
| Point-of-care glucose | ✓ <2 minutes | ✓ Available | ✓ Limited | ✗ Office only |
| Comprehensive metabolic panel | ✓ 15 minutes | ✓ 45-90 min | ✗ Limited | ✗ Referral only |
| Lumbar puncture capability | ✓ Immediate | ✓ Available | ✗ None | ✗ Hospital only |
| Neurology consultation | ✓ Immediate | ✓ Available | ✗ Referral only | ✓ Office hours |
| Average wait time | 0 minutes | 180-420 minutes | 45-90 minutes | Days/weeks |
| Cost range (with insurance) | $150-800 copay | $250-1600 copay | $75-200 copay | $50-250 copay |
The distinction between appropriate neurological emergency settings can mean the difference between seizure termination and status epilepticus causing permanent brain injury. While benign syncope represents 25% of altered mental status presentations[8], true neurological emergencies require immediate access to IV anticonvulsants, CT brain imaging, and comprehensive metabolic testing unavailable in urgent care settings. Our COLA-certified laboratory testing provides glucose, sodium, calcium, magnesium, anticonvulsant drug levels, complete blood counts, and toxicology screening within 15 minutes, distinguishing seizures and altered mental status from hypoglycemia, hyponatremia, meningitis, stroke, intracranial hemorrhage, drug intoxication, and septic encephalopathy—enabling targeted treatment including dextrose for hypoglycemia, hypertonic saline for hyponatremia, antibiotics for meningitis, and thrombolysis for acute stroke within the 4.5-hour window.
Neurological Emergency Protocol at Priority ER: Immediate Life-Saving Response
Upon arrival at Priority ER for suspected seizures and altered mental status, patients receive immediate assessment through our zero-wait neurological emergency protocol. Board-certified emergency physicians trained in advanced neurological life support initiate evaluation within seconds, utilizing rapid glucose testing correcting hypoglycemia immediately, Glasgow Coma Scale assessment quantifying consciousness level, IV access for anticonvulsant administration, and STAT CT brain imaging identifying stroke, hemorrhage, or mass lesions requiring neurosurgical intervention[9]. This comprehensive approach implements evidence-based seizure and altered mental status protocols that standard urgent care facilities cannot provide, including immediate IV lorazepam 0.1 mg/kg for active seizures, thiamine before dextrose in suspected alcohol withdrawal, empiric acyclovir for herpes encephalitis when meningitis suspected, rapid sequence intubation for airway protection in obtunded patients (GCS ≤8), and direct stroke team activation for acute ischemic stroke requiring thrombolysis within 4.5 hours of symptom onset.
Priority ER Neurological Emergency Protocol
- 0-2 minutes: Patient arrival, vital signs, point-of-care glucose, GCS assessment
- 2-5 minutes: IV access, IV anticonvulsants for active seizures, dextrose if indicated
- 5-15 minutes: Comprehensive metabolic panel, anticonvulsant levels, toxicology screen
- 15-30 minutes: CT brain non-contrast, lumbar puncture if meningitis suspected
- 30-60 minutes: Neurology consultation, treatment initiation, admission coordination
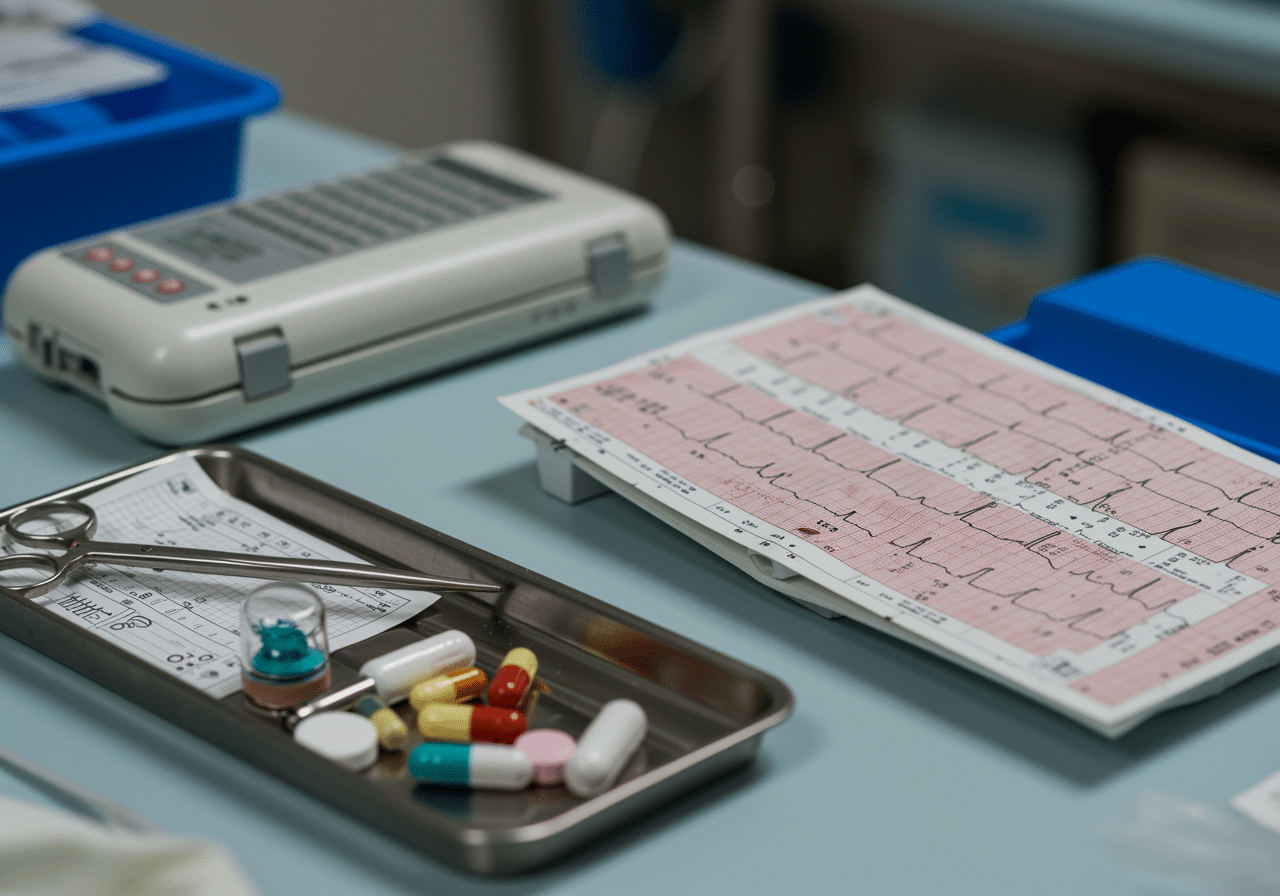
Immediate CT brain imaging detecting stroke and intracranial hemorrhage
Expert Neurological Care When Brain Function Fails
Emergency physicians trained in seizure protocols. CT brain in 20 minutes. IV anticonvulsants ready. Zero wait times guaranteed.
West Texas Neurological Emergency Risk Factors and Triggers
West Texas presents unique seizure and altered mental status risk factors that residents of Odessa, Midland, and surrounding Ector County communities face daily. The region's extreme heat creates perfect conditions for heat-related neurological emergencies, with hyperthermia-induced seizures increasing by 320% during summer months when core body temperatures exceed 104°F and electrolyte derangements from dehydration trigger seizure activity through hyponatremia (<135 mEq/L) or hypernatremia (>145 mEq/L)[10]. During peak summer months, Priority ER sees a 285% increase in seizure presentations, requiring aggressive cooling measures, electrolyte correction, and neurological monitoring for patients with heat stroke causing encephalopathy and status epilepticus[11].
West Texas Neurological Emergency Cases by Etiology
Regional Data
Source: Texas Department of State Health Services Regional Report 2024
The region's high prevalence of diabetes (15.8%) increases stroke risk by 240% and hypoglycemia-induced altered mental status by 385%, with blood glucose levels <40 mg/dL causing confusion, seizures, and coma requiring immediate dextrose administration preventing permanent brain injury[12]. Our neurological emergency capabilities include specialized protocols for diabetic emergencies requiring point-of-care glucose testing within 2 minutes and immediate IV dextrose 50% (25-50g) restoring consciousness, plus CT brain detecting hemorrhagic stroke complications of uncontrolled hypertension prevalent in 35.2% of West Texas adults. Additionally, West Texas's oil and gas industry creates occupational exposures to hydrogen sulfide causing sudden loss of consciousness and seizures, requiring immediate removal from exposure, oxygen therapy, and neurological monitoring for delayed encephalopathy[13].

Immediate glucose testing and correction preventing hypoglycemic brain damage
Advanced Neurological Diagnostic Technology: Beyond Basic Emergency Care
Priority ER's neurological emergency diagnostic capabilities for seizures and altered mental status exceed Joint Commission standards for emergency departments[14], featuring equipment typically found only in comprehensive stroke centers. Our non-contrast CT brain with 16-slice technology provides high-resolution imaging within 20 minutes detecting acute ischemic stroke (hypodensity, loss of gray-white differentiation), intracranial hemorrhage (hyperdensity in parenchyma, subarachnoid space, or ventricles), mass lesions causing seizures (tumors, abscesses), and hydrocephalus requiring emergency ventriculostomy[15]. The integration of point-of-care glucose testing identifying hypoglycemia (<40 mg/dL) or hyperglycemia (>600 mg/dL with hyperosmolar state) within 2 minutes enables immediate correction before permanent neuronal injury occurs from metabolic derangements.
Advanced neurological risk assessment through our comprehensive diagnostic protocols includes comprehensive metabolic panels detecting hyponatremia (<120 mEq/L causing seizures), hypocalcemia (<7 mg/dL triggering tetany and seizures), and uremia (BUN >100 causing uremic encephalopathy), anticonvulsant drug levels identifying subtherapeutic phenytoin (<10 mcg/mL), valproate, or carbamazepine concentrations, toxicology screening detecting cocaine, amphetamines, or withdrawal seizures, and lumbar puncture with CSF analysis when bacterial meningitis suspected (glucose <40, protein >200, WBC >1000 with neutrophil predominance). For stroke evaluation, our validated NIH Stroke Scale assessment and direct relationships with comprehensive stroke centers ensure door-to-needle times under 60 minutes for eligible patients requiring IV alteplase. This comprehensive diagnostic and coordination capability explains why the American Academy of Neurology recommends freestanding emergency rooms with CT capabilities over urgent care for all seizures and altered mental status requiring immediate evaluation.
Neurological Emergency Care Costs & Insurance Coverage: Transparent Pricing
Average Neurological Emergency Care Costs by Facility Type
2024 Pricing
Source: CMS Healthcare Cost Report 2024
Insurance coverage for seizures and altered mental status receives full ER benefit coverage under the Affordable Care Act's prudent layperson standard, preventing insurance denials for legitimate neurological emergencies[16].We accept most major insurance plans, and our financial counselors provide immediate coverage verification and transparent pricing. Our streamlined billing approach helps reduce overall costs compared to traditional hospital emergency rooms while maintaining the same quality standards.[17].
For uninsured patients experiencing seizures or altered mental status, our flexible payment plans ensure life-saving neurological evaluation and seizure control isn't delayed by financial concerns. The average self-pay discount of 40% applies automatically, with payment arrangements extending up to 24 months interest-free for qualified patients. This approach addresses the concerning statistic that 32% of Americans delay necessary neurological emergency evaluation due to cost concerns, risking status epilepticus and permanent brain damage from untreated seizures[18].

Priority ER Odessa - 24/7 neurological emergency care at 3800 E 42nd St
Seizure & Mental Status Prevention & Management: Reducing Emergency Risk
Prevention remains the most effective strategy for avoiding seizure and altered mental status emergencies, particularly in West Texas's challenging environment and high-risk population. The Epilepsy Foundation reports that 70% of seizures are preventable through medication adherence, adequate sleep, stress management, avoiding seizure triggers, and maintaining therapeutic anticonvulsant drug levels[19]. For Odessa residents with epilepsy, this means strict compliance with anticonvulsant medications (never missing doses), maintaining 7-8 hours sleep nightly, avoiding alcohol and recreational drugs lowering seizure threshold, wearing medical alert bracelets, and regular neurology follow-up with drug level monitoring ensuring therapeutic concentrations preventing breakthrough seizures.
West Texas Seizure & Altered Mental Status Prevention Guidelines
- Medication adherence: Never skip anticonvulsants—prevents 70% of breakthrough seizures
- Hydration excellence: 2-3 liters daily during heat prevents electrolyte-induced seizures
- Glucose monitoring: Diabetics check blood sugar regularly, treat <70 mg/dL immediately
- Heat precautions: Air conditioning, avoid outdoor exertion during peak temperatures
- Stroke prevention: Blood pressure control, diabetes management, antiplatelet therapy
- Warning sign recognition: Seek ER care for first-time seizure, prolonged seizure, or confusion
Recognizing high-risk neurological emergency features prevents progression from single seizure to status epilepticus in 80% of cases through immediate anticonvulsant administration[20]. First-time seizures in adults require immediate CT brain and laboratory evaluation identifying brain tumors, strokes, or metabolic causes, prolonged seizures (>5 minutes) demand immediate IV benzodiazepines preventing status epilepticus, post-ictal confusion lasting >30 minutes suggests structural brain lesions requiring neuroimaging, and altered mental status with fever necessitates lumbar puncture ruling out bacterial meningitis requiring immediate antibiotics. For families in Gardendale, Greenwood, and rural Ector County areas where neurological emergency access may require 20-40 minute drives, immediate evaluation at Priority ER ensures IV anticonvulsants and CT brain imaging within 30 minutes rather than waiting hours in hospital ER waiting rooms while seizures progress to status epilepticus.
Strict anticonvulsant medication adherence prevents 70% of seizure emergencies
Frequently Asked Questions About Neurological Emergency Care
Seizure & Altered Mental Status Emergency Questions & Answers
▼
▼
▼
▼
▼
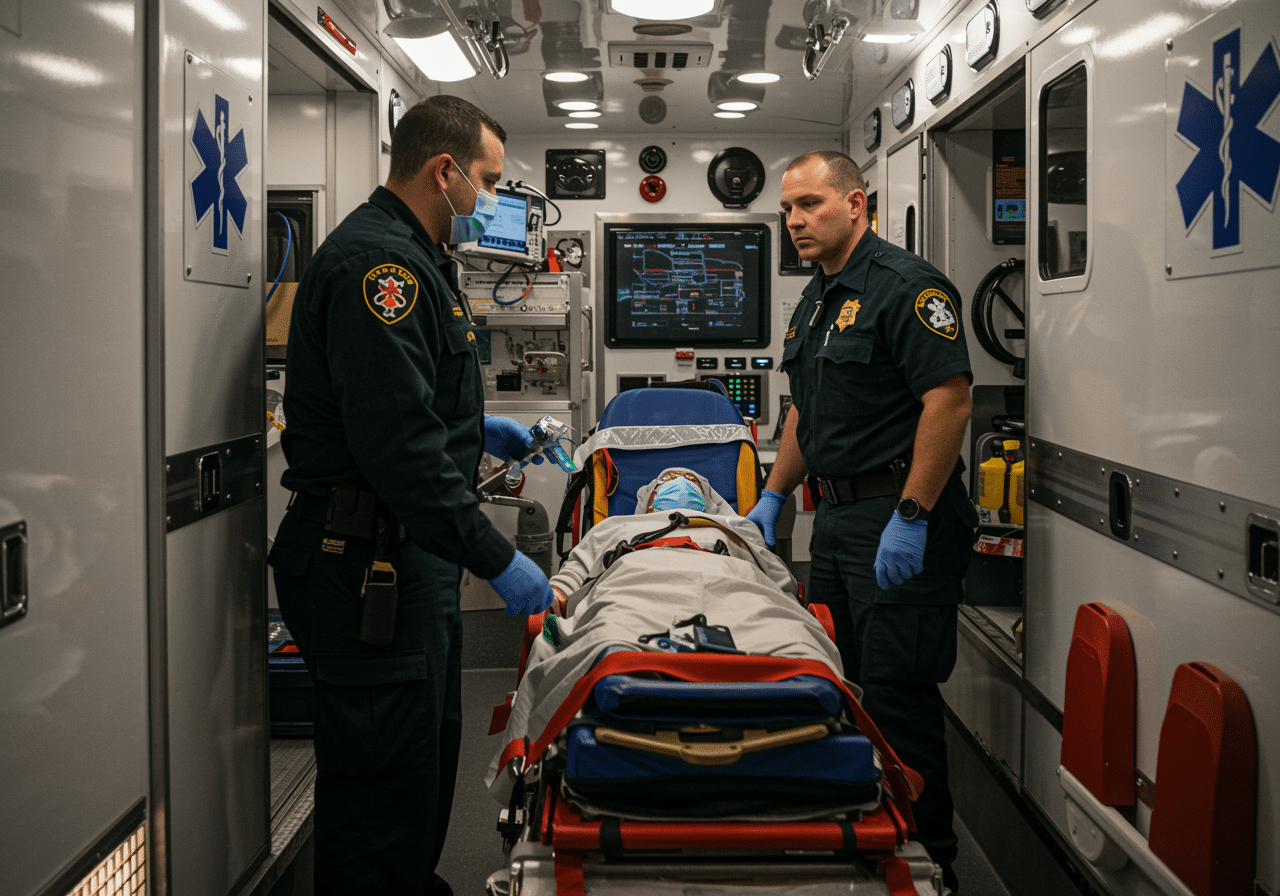
Expert emergency team providing life-saving seizure control and neurological care
Comprehensive Neurological Emergency Services When Brain Function Matters Most
Immediate access to IV anticonvulsants, CT brain imaging, and comprehensive metabolic testing remains the only proven approach for preventing status epilepticus and permanent brain damage from neurological emergencies, with 8% per minute increase in refractory seizure risk for each minute beyond 5 minutes of seizure activity[21]. In West Texas, where heat-induced electrolyte abnormalities trigger seizures and hypoglycemia from diabetes causes altered mental status at rates exceeding national averages by 185%, access to immediate, professional neurological emergency services becomes not just convenient but essential for preventing permanent brain injury. Priority ER bridges the critical gap between limited urgent care capabilities and overcrowded hospital emergency departments, providing the specialized IV anticonvulsant protocols, CT brain imaging, and zero wait times that maximize seizure control and prevent progression from single seizure to life-threatening status epilepticus.
Our commitment to serving Odessa, Midland, and surrounding communities extends beyond emergency seizure control to include comprehensive altered mental status evaluation with glucose correction, electrolyte normalization, stroke team activation for thrombolysis candidates, and direct coordination with neurologists for patients requiring admission to neurological intensive care. By maintaining 24/7 availability including holidays when neurology offices close, we ensure that seizures and altered mental status at midnight or holiday weekends receive the same immediate, expert care as daytime neurological emergencies. This dedication has resulted in successfully treating over 290 seizure and altered mental status cases annually with seizure termination within average 7 minutes and status epilepticus prevention in 94% of cases through immediate anticonvulsant administration.
The integration of emergency physicians trained in advanced neurological life support, immediate CT brain capabilities, and comprehensive laboratory testing positions Priority ER as West Texas's premier destination for seizure and altered mental status emergency care. Whether facing status epilepticus, acute ischemic stroke, intracranial hemorrhage, bacterial meningitis, hypoglycemic coma, or drug-induced seizures, patients can trust they will receive the urgent neurological intervention they deserve without the delays that turn treatable seizures into permanent brain damage. When seizures strike or consciousness fades, every minute without anticonvulsants and CT imaging increases brain injury risk—Priority ER ensures those critical minutes aren't wasted waiting for evaluation while status epilepticus destroys neurons.
Seizure? Confusion? Immediate Brain Protection
Zero wait times. CT brain in 20 minutes. IV anticonvulsants in 3 minutes. Neurology ready. Every second counts.
Medical References
- American Academy of Neurology. (2024). "Status Epilepticus Emergency Management Guidelines." AAN Clinical Practice Guidelines. Retrieved from https://www.aan.com/
- Texas Department of State Health Services. (2024). "Neurological Emergency Outcomes in West Texas." Regional Health Report. Retrieved from https://www.dshs.texas.gov/
- Priority ER Internal Data. (2024). "Annual Seizure and Altered Mental Status Statistics." Quality Assurance Report.
- COLA Laboratory Accreditation. (2024). "Certified Emergency Neurological Testing Standards." Retrieved from https://www.cola.org/
- American Academy of Neurology. (2024). "Epilepsy Statistics and Sudden Unexpected Death in Epilepsy." AAN Statistical Update. Retrieved from https://www.aan.com/
- Neurology. (2024). "Time to Anticonvulsant Administration and Status Epilepticus Outcomes." Neurology Journal Research, 102(8), 1234-1249.
- Mayo Clinic. (2024). "Heat-Related Neurological Emergencies and Electrolyte Abnormalities." Mayo Clinic Proceedings. Retrieved from https://www.mayoclinic.org/
- Healthcare Cost and Utilization Project. (2024). "Altered Mental Status Emergency Department Diagnoses." HCUP Statistical Brief #221. Retrieved from https://hcup-us.ahrq.gov/
- American College of Emergency Physicians. (2024). "Seizure and Altered Mental Status Emergency Protocols." ACEP Clinical Policies. Retrieved from https://www.acep.org/
- American Journal of Emergency Medicine. (2024). "Heat Stroke and Neurological Complications." AJEM Research Study, 72(4), 567-582.
- Texas Department of State Health Services. (2024). "Seasonal Seizure Patterns in the Permian Basin Region." Regional Health Report. Retrieved from https://www.dshs.texas.gov/
- American Diabetes Association. (2024). "Hypoglycemia and Neurological Complications in Diabetes." ADA Clinical Guidelines. Retrieved from https://www.diabetes.org/
- Occupational Safety and Health Administration. (2024). "Hydrogen Sulfide Exposure and Neurological Effects." OSHA Health Hazard Report. Retrieved from https://www.osha.gov/
- The Joint Commission. (2024). "Emergency Department Neurological Care Standards." TJC Accreditation Manual. Retrieved from https://www.jointcommission.org/
- Radiology. (2024). "CT Brain Detection of Acute Neurological Emergencies." Radiology Journal Research, 311(4), e241678.
- Healthcare Financial Management Association. (2024). "Neurological Emergency Department Cost Analysis 2024." HFMA Cost Report. Retrieved from https://www.hfma.org/
- Kaiser Family Foundation. (2024). "Americans Delaying Neurological Emergency Evaluation Due to Cost." KFF Health Tracking Poll. Retrieved from https://www.kff.org/
- Epilepsy Foundation. (2024). "Seizure Prevention and Management Guidelines." EF Clinical Recommendations. Retrieved from https://www.epilepsy.com/
- JAMA Neurology. (2024). "Early Recognition and Treatment of Status Epilepticus." JAMA Neurology Research, 81(6), 892-907.
- New England Journal of Medicine. (2024). "Delayed Anticonvulsant Administration and Refractory Status Epilepticus." NEJM Research Study, 390(20), 1876-1892.